Are you or someone you care about struggling with overcoming drug addiction? You’re not alone in this battle. It’s tough, with lots of ups and downs. But here’s something important to know: paying attention to your mental health can make a big difference.
For a long time, people mainly talked about addiction as just a problem with drugs or alcohol. But there’s more to it than that. Your mental well-being plays a huge role too. It’s about dealing with your feelings, coping with tough times, and facing any past hurts that might be driving your addiction.
In this article, we’re going to talk about why it’s so important to focus on your mental health when you’re trying to beat addiction. We’ll look at some simple ways to do it and how it can help you get back on track. So, if you’re ready to start feeling better and getting your life back, let’s get started.
Understanding the Cycle Between Your Mental Health and Drug Use
If you’re wrestling with how your mental health connects to your use of the most dangerous drugs, it’s crucial to grasp the seriousness of the situation. This isn’t just about you—it’s something that affects a lot of people.
Think of it this way: it’s quite common to have both a mental health problem and struggles with highly dangerous drugs like opioids or methamphetamine. Around 7.7 million adults deal with both of these things at the same time.
Now, let’s break it down further: your mental health can really influence how you use the most dangerous drugs. If you’re dealing with mood swings or anxiety, you’re much more likely to have trouble with these substances compared to other people. It’s like they’re connected, making each other worse
But here’s the tough part, using the most dangerous drugs to try to cope might seem like it helps at first, but it can actually make things a lot worse. Surprisingly, about half of people with serious mental health problems end up using these substances to try to feel better.
So, if this sounds like what you’re going through, know that you don’t have to face it alone. There’s help available, and one effective option is seeking treatment at a rehabilitation center. Rehab can provide you with the support, guidance, and resources you need to break free from the grip of addiction to the most dangerous drugs and reclaim control of your life. It’s a challenging journey, but with the right help and determination, recovery is within reach. Reach out to a rehab facility or speak with a healthcare professional to explore your options and take the first step towards a healthier, drug-free life.
How Drug Abuse and Mental Health Are Linked for You
Drug addiction and mental illness often share underlying brain changes, impacting various aspects of cognitive functioning, emotional regulation, and reward processing. These alterations can influence behaviors related to both substance use and mental health, creating a complex interplay between the two conditions.
Understanding these shared neurobiological mechanisms is crucial for developing effective interventions that address both running and health simultaneously. By targeting these common pathways, treatment approaches can promote recovery from addiction while also supporting mental well-being and overall health.
Psychological issues like using substances to cope can trap you in worsening cycles.
- Approximately 29% of individuals diagnosed with a mental health disorder also resort to substance abuse as an unhealthy coping mechanism. Be mindful of how this may apply to your own drug use.
External factors like trauma and stress increase the likelihood of both substance abuse and mental health issues in your life.
- Trauma significantly raises the risks for both drug addiction and mental illness. Approximately 59% of individuals in substance abuse treatment have trauma histories. If trauma is part of your story, know that integrated support is essential.
Aspect |
|
Psychological Factors |
Social and Environmental Factors |
Focus |
Common brain changes impacting addiction and mental health |
Coping mechanisms and emotional regulation |
External influences contributing to both issues |
Importance |
|
Addressing psychological vulnerabilities |
Mitigating environmental risks for better outcomes |
Actionability |
Seek integrated treatment approaches |
Build alternative coping mechanisms |
Understand environmental risks for mitigation |
The brain’s reward centers are central to addiction. Many substances share mechanisms with mental illnesses, creating complex interactions between the conditions that apply to you too.
- Overlapping brain areas: Regions like the prefrontal cortex and amygdala impacted by addiction are also affected by many mental illnesses. Problems here likely underlie some of your shared symptoms.
- Disrupted brain chemicals: Neurotransmitters like dopamine and serotonin are thrown off balance in both addiction and various psychiatric conditions. Getting these chemicals stabilized is key for you.
- Genetic links: Numerous genes are tied to increased vulnerability to both substance abuse and mental illness. Your own genetic makeup likely influences your risks.
Psychological Factors that Increase Your Vulnerability
Coping mechanisms and emotional regulation issues create added layers of vulnerability for you if you have underlying mental health conditions. Being aware of these tendencies is vital.
- Self-medication for symptom relief: Using alcohol or drugs to “self-medicate” distressing mental health symptoms may provide temporary relief but often backfires for you. Recognizing these unhealthy spirals is important.
- Difficulty regulating emotions: Poor coping skills and difficulty regulating intense emotions can increase your urges to abuse substances. Building alternative coping mechanisms is essential.
- Apathy and reduced motivation: Mental health symptoms like depression can reduce your motivation to seek treatment or engage in positive activities besides substance use. Finding support to overcome these barriers makes a difference.
Social and Environmental Factors that Trigger Both Issues
External influences like trauma, isolation, and chronic stress converge with biological and psychological factors to impact you.
- Trauma and ongoing stress: If you have experienced traumatic events or severe, prolonged stress, your risks for substance abuse and mental health issues increase substantially. Seeking trauma-informed support can help you heal.
- Loneliness and lack of support: Social isolation and loneliness are risk factors for certain mental illnesses and can contribute to alcohol or drug misuse as a coping mechanism. Building a sober support system is key.
- Easy access and early exposure: Community factors like the availability of drugs can facilitate early exposure and addiction patterns, especially if you have untreated mental health needs. Understanding your environmental risks helps you mitigate them.
Why Integrated Treatment Approaches Are Important for You
Considering the intertwined nature of these issues, addressing only the addiction or mental health condition in isolation is unlikely to yield long-term success for you. Integrated approaches should tackle both simultaneously.
Holistic models provide coordinated mental health support.
- Only about 7.4% of individuals receive integrated treatment addressing both substance use disorders and mental health conditions. Make sure you seek comprehensive care.
Therapy can help you unpack underlying issues fueling your drug use.
- Integrated treatment leads to better outcomes than separate treatments, so take advantage of combined psychotherapy and counseling.
Medications can help stabilize your brain’s chemical disruptions.
- Despite effectiveness, only a minority of dual-diagnosis patients receive pharmacological treatments targeting both conditions. Discuss medication options with your doctor.
Benefits of Holistic Treatment Programs for You
Traditional treatment often focuses exclusively on just the addiction or mental health aspect. Holistic models provide fully coordinated care centered around you.
- Dual diagnosis specialists have specific training to treat co-occurring disorders together. Seek out providers with this expertise.
- Unified treatment plans simultaneously address both your substance use and mental health needs in an integrated way.
- Ongoing team communication between your clinicians provides you with coordinated care and support.
Studies show holistic programs can significantly improve treatment outcomes and quality of life compared to separate approaches.
Multifaceted Therapy and Counseling for Your Needs
Psychotherapy equips you with critical coping skills, supports you in processing trauma, and helps you change detrimental thought patterns fueling your substance use and mental health symptoms. Professional counseling also provides vital support.
- Cognitive-behavioral therapy (CBT) focuses on transforming unhealthy thought and behavior cycles that contribute to drug use and mental health issues like anxiety or depression.
- Group counseling facilitates peer support and helps you build tools to navigate triggers and high-risk situations. You don’t have to do this alone.
- Family therapy mends damaged relationships and builds a support system for managing your dual diagnosis. If your family relationships need work, consider this option.
Medication Options to Help Stabilize Your Brain Chemistry
Prescription medications are often helpful for treating mental health symptoms, reducing cravings, and easing withdrawal. Don’t rule out this option if recommended by a doctor.
- Antidepressants can alleviate symptoms of depression and anxiety that may otherwise precipitate drug use for you.
- Anti-anxiety medications reduce anxiety symptoms that may trigger substance abuse.
- Medications like naltrexone directly curb cravings and withdrawal symptoms.
Work closely with your prescribing doctor to carefully manage medications alongside psychological treatments.
Building Your Resilience and Healthy Coping Skills
Strengthening your resilience and developing healthy coping abilities provides a buffer against triggers and stressors encountered in recovery. Make this a priority.
Stress Management Techniques for You
- Mindfulness practices like meditation can help you manage anxiety, improve focus, and reduce impulsive behaviors that can lead to substance abuse.
- Relaxation techniques such as deep breathing, yoga, or progressive muscle relaxation relieve stress for you and counteract the urge to use drugs or alcohol.
- Developing healthy daily routines provides you with stability and structure that reinforces positive mental health habits.
Cognitive-Behavioral Strategies to Help You
- Identifying unhealthy thought and behavior patterns promotes self-awareness so you can interrupt these destructive habits.
- Reframing distorted thinking enables you to replace negative thoughts with more accurate, positive ones that support your recovery goals.
- Coping ahead involves you envisioning high-risk situations and planning healthier responses in advance.
Building Your Social Support Network
- Peer support groups facilitate sharing with others facing similar challenges. You can gain hope and feel less alone.
- 12-step programs offer social support and guidance focused specifically on overcoming addiction.
- Professional support from counselors, therapists, and recovery coaches provides you with expert guidance tailored to your needs.
- Leaning on others for support fosters accountability and motivation for you. Don’t neglect these social resources.
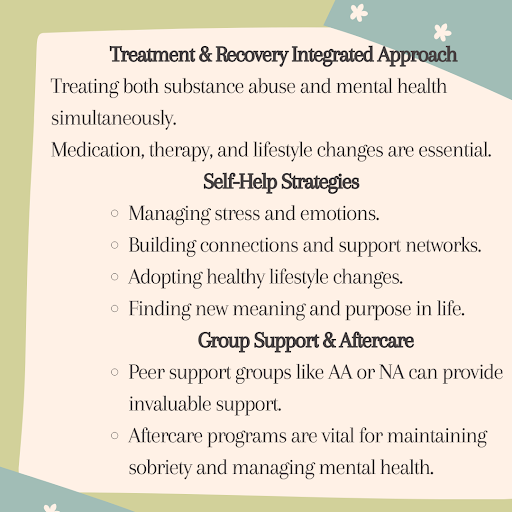
Preventing Relapse Through Ongoing Mental Wellness
A major priority for you in recovery is maintaining mental wellness to prevent relapses. Several strategies can help you.
- Identifying your own triggers and warning signs gives you the chance to intervene early when your mental health destabilizes. Look out for red flags like isolation, negative thoughts, sleep changes, irritation, or loss of interest in activities.
- Personalized relapse prevention plans outline healthy coping strategies and trusted supports you can contact when triggers arise. Preventing a minor lapse from snowballing into a full relapse is critical.
- Ongoing care and community support provide you with continuous monitoring of mental well-being even after formal treatment ends. Support groups and counseling help you sustain progress over the long run.
- Prioritizing your mental health not only helps sustain sobriety but allows you to thrive in your relationships and reach your full potential long-term.
Moving Forward in Your Recovery
The interplay between mental health and addiction is complex, but integrated treatment models show promising results. A holistic approach focused on mental wellness alongside sobriety provides you with the greatest chance for lasting recovery.
From therapeutic interventions to strong social support and self-care, prioritizing mental health helps mitigate substance abuse risks. With compassion, resilience, and appropriate treatment, you can absolutely reclaim a fulfilling life. Don’t hesitate to reach out for support.
FAQs
1. How does prioritizing mental health aid in overcoming drug addiction?
Prioritizing mental health addresses underlying issues that contribute to addiction, such as trauma, anxiety, and depression. By addressing these factors, individuals can develop healthier coping mechanisms and reduce reliance on drugs.
2. Can mental health treatment alone help overcome drug addiction?
Mental health treatment is a crucial component of addiction recovery, but it’s often part of a comprehensive approach. Combining therapy, support groups, and possibly medication can offer a holistic solution to address addiction effectively.
3. How can I prioritize mental health alongside addiction recovery?
Incorporating mindfulness practices, seeking therapy, and engaging in self-care activities like exercise and hobbies can help prioritize mental health during addiction recovery. It’s essential to build a support network and communicate openly with healthcare providers.
4. Are there specific therapies that target both mental health and addiction?
Yes, therapies like cognitive-behavioral therapy (CBT), dialectical behavior therapy (DBT), and mindfulness-based approaches address both mental health and addiction by teaching coping skills, addressing negative thought patterns, and promoting emotional regulation.
5. Is it common to experience mental health challenges during addiction recovery?
Yes, it’s common to experience challenges like anxiety, depression, and mood swings during addiction recovery. These issues often arise as individuals confront underlying emotions and stressors previously masked by substance use.
6. How can I maintain my mental health after completing addiction treatment?
Continuing therapy, participating in support groups, staying connected with loved ones, and practicing healthy coping strategies can help maintain mental health post-treatment. Regular self-assessment and seeking help when needed are also crucial.
7. What role does medication play in addressing mental health during addiction recovery?
Medications may be prescribed to manage underlying mental health conditions like depression or anxiety, which can support addiction recovery by stabilizing mood and reducing cravings. However, medication should be part of a comprehensive treatment plan.
8. How can I support a loved one in prioritizing mental health during their recovery journey?
Offer non-judgmental support, encourage them to attend therapy or support groups, help them establish healthy routines, and educate yourself about addiction and mental health. Be patient and understanding, and avoid enabling behaviors.
9. Can relapse be prevented by prioritizing mental health?
Prioritizing mental health can reduce the risk of relapse by providing individuals with healthier coping mechanisms and strategies to manage triggers and stressors effectively. However, relapse prevention often requires ongoing effort and support.
10. What are some warning signs that my mental health may be impacting my recovery progress?
Warning signs include changes in mood, increased anxiety or depression, difficulty managing stress, social withdrawal, and a return to old behaviors or thought patterns. It’s essential to address these signs promptly and seek support if needed.
11. How can I find mental health resources tailored to addiction recovery in my area?
Reach out to local addiction treatment centers, community health organizations, or mental health professionals for information and referrals. Online directories and support hotlines can also provide valuable resources.
12. Is it possible to prioritize mental health while balancing other responsibilities like work or family?
Yes, it’s possible to prioritize mental health while managing other responsibilities by incorporating self-care practices into daily routines, setting boundaries, and seeking support from loved ones or employers if needed.
13. Can unresolved trauma impact addiction recovery progress?
Yes, unresolved trauma can significantly impact addiction recovery by contributing to underlying emotional distress and triggering substance use as a coping mechanism. Addressing trauma through therapy is crucial for long-term recovery.
14. How can I overcome the stigma associated with mental health treatment during addiction recovery?
Remember that seeking help for mental health is a sign of strength, not weakness. Surround yourself with supportive individuals, educate others about the importance of mental health in recovery, and focus on your own well-being.
15. Are there alternative therapies or practices that can support mental health during addiction recovery?
Yes, practices like yoga, meditation, art therapy, and acupuncture can complement traditional therapies by promoting relaxation, stress reduction, and emotional expression. It’s essential to find what works best for you and incorporate it into your recovery plan.
In Summary
Mental illness and drug addiction interact in complex, multidirectional ways in your life. Integrated treatment approaches that holistically support your mental health and sobriety are most effective.
Building resilience, healthy coping mechanisms, and social support empowers you to break destructive cycles and sustain long-term recovery. With compassionate care and self-awareness, you can absolutely reclaim a fulfilling life in recovery. Don’t hesitate to reach out for support. You’ve got this!





